TADH breast specialists understand the anxiety associated with a breast concern and aim to provide rapid turnaround times.
Services at TADH include OBSP screening examinations, High Risk screening OBSP, diagnostic mammography for palpable breast lesions, breast pain, nipple discharge, skin changes, screening as well as diagnostic ultrasound, MRI and interventional procedures. A referral from your Health Care Provider (HCP) is necessary except for OBSP.
At TADH we offer:
• Accredited full-service screening and diagnostic digital mammography
• OBSP (Ontario Breast Screening Program)
• High Risk OBSP
• Screening and Diagnostic Mammography
• Stereotaxic biopsy
• Breast Ultrasound (US)
• US guided fine needle aspirations
• US guided core biopsies
• Breast Magnetic Resonance Imaging (MRI)
• MRI guided vaccum assisted biopsies
• Galactography
• Pre-operative needle localizations
• Lumpectomies
• Mastectomies
• Sentinel node biopsies
• Rapid turnaround for biopsy scheduling and availability of results
• Subspecialist Radiologist with expertise in breast imaging and intervention
• Expert pathology interpretation is provided through University Health Network (UHN) in Toronto
• Referral to one of the TADH breast surgeons
Ontario Breast Screening Program (OBSP)
The Ontario Breast Screening Program (OBSP) is a program of Cancer Care Ontario. OBSP provides top-quality breast screening services for women 50+ who have no previous history of breast cancer. OBSP offers important advantages for women and their primary care providers, including recruitment, recall and follow-up and ongoing quality assurance. All OBSP sites are accredited by the Canadian Association of Radiologists Mammography Accreditation Program.
OBSP sites help women with an abnormal screen to move through the diagnostic phase. The program is free of charge and accessible without a physician referral. Results of screening through OBSP are available within two weeks to both the patient & doctor. OBSP will also set up extra tests or referrals if necessary. A letter of reminder is sent out to patients when it is time for the next screening mammogram (usually 2 years).
Women who fit the OBSP criteria can self refer or have their Health Care Provider (HCP) refer them to the program.
You must:
- Have a valid Ontario Health Card
- Be a resident of Ontario
- Be 50 years of age or older
- Have no acute breast symptoms (e.g. no masses, no breast discharge)
- Have no history of breast cancer
- Have not had a mammogram in the last 12 months
- Have no breast implants now
Our vision is to provide patients with the most advanced technology, wherever possible, to improve the individual experience. Digital technology allows TDH to achieve that vision.
For more information about the Timmins and District Hospital Mammography program, or to book an appointment, please call bookings at (705) 360-6012.
For additional information visit: Cancer Care Ontario
High Risk Ontario Breast Screening Program
On July 1, 2011, the Ontario Breast Screening Program (OBSP) expanded services to include screening of women aged 30 to 69 at high risk of developing breast cancer. Women who think they may be at high risk should visit their family physician for a referral to the OBSP. Referrals will be based on specific criteria, such as genetics and family or medical history.
Women at high risk for breast cancer can receive annual breast MRI or bilateral breast ultrasound and mammography screening as part of the Ontario Breast Screening Program (OBSP).
Learn more about who is eligible for the high risk screening program.
For additional information visit: Cancer Care Ontario
How to Refer a Patient
To refer a patient to the high-risk breast screening program at TDH:
1. Complete a Requisition for High Risk Screening by a physician
2. Fax the completed form to (705) 360-6681
Contact Information
Tina Bilodeau, MRT(R)
Coordinator of Breast Imaging Services / Patient Navigator
(705) 267-2131 ext. 2246
Mammography
Mammography is a screening and diagnostic examination that looks for breast cancer and other abnormalities. A mammogram can detect masses, changes in breast tissue and calcifications. A woman's first mammogram is called a baseline mammogram. All future mammograms are compared to prior studies.
A specially trained radiology technologist performs mammograms. During a mammogram, the breast is appropriately positioned and compressed. Usually two images are taken of each breast, from different angles. Compression may be uncomfortable for a few seconds while the X-ray is taken. Some women may feel sore after a mammogram. Compression is important in obtaining good quality images.
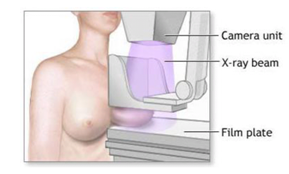
If necessary, additional mammogram images, an ultrasound scan or, in special situations, a magnetic resonance (MR) scan of the breast may need to be arranged. In this case our department staff will contact you with a call back appointment. Recalls will be arranged in the timeliest manner possible.
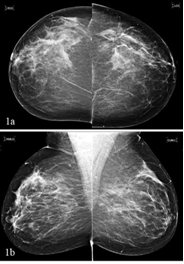
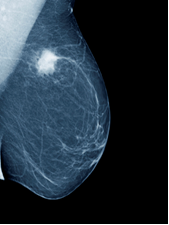
Routine 4 view digital mammogram Breast Cancer
Galactorgraphy
Galactography (also known as ductography) is a test used to evaluate the cause of discharge. This examination is performed if a woman experiences leakage from the nipple and if the fluid is bloody, clear or yellowish in color. For this procedure a tiny blunt end needle is dropped into the duct and a small amount of dye is injected. Following this, a mammogram is performed to evaluate the duct.

Breast Ultrasound
Ultrasound is used to evaluate a finding detected on mammography or to assess an area of clinical concern. A lesion can be a cyst (fluid-filled sac) or a solid tumor (either benign or malignant). Screening Ultrasound may be performed in women with dense breasts or high risk.
Ultrasound involves the use of sound waves to create a picture of the breast. Ultrasound is painless. During the procedure a transducer is moved along the skin of the breast.

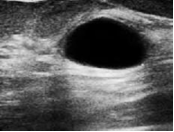
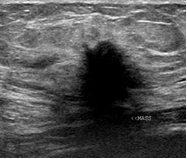
Cyst Cancer
Magnetic Resonance
Breast magnetic resonance (MR) imaging is used in screening of high risk patients, and as a diagnostic study to help evaluate a finding detected on mammography or ultrasound and in certain pre-operative cases. MRI is also used to assess breast silicone implants.
MR imaging involves the use of magnets and computers to create images of areas inside the body. A computer compiles hundreds of images from each MR scan. Each image shows a thin, horizontal slice of breast tissue. The patient is scanned in a face down position. IV is inserted prior to scanning.

During breast MR examinations, use of a contrast dye provides detailed images of the breast. MR scans reveal masses, both benign and malignant. No contrast dye is necessary for evaluating the implants.
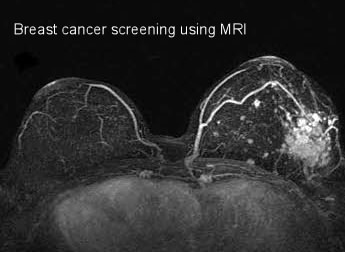
If a suspicious area is detected, you may be recalled for an ultrasound, additional mammogram examination or MRI guided biopsy.
Breast Biopsy
A biopsy may be required if:
- You or your doctor feels a lump or thickening in your breast
- Your mammogram shows a suspicious area in your breast
- An ultrasound scan reveals a suspicious finding
- An MRI scan reveals a suspicious finding
- You have unusual nipple changes, including crusting, scaling, dimpling skin or bloody discharge
How you prepare
Please let us know if you have any allergies, or are taking blood thinners.
A breast biopsy is considered the best way to evaluate a suspicious area in your breast to determine if it is breast cancer. A breast biopsy provides a sample of tissue for laboratory testing. The samples of cells or tissues taken are sent to a laboratory for analysis by expert pathologists at University Health Network (UHN) in Toronto. A breast biopsy can help determine whether or not you need additional surgery or other treatment. There are several different types of breast biopsy procedures.
Fine-needle aspiration
This is the simplest type of breast intervention and may be used to evaluate a lesion detected on mammography or ultrasound. For the procedure, you lie on a bed, and then under ultrasound guidance, the radiologist will locate the lesion and will administer local anesthetic (freezing of the skin). The radiologist will use a very fine needle to insert into the lesion (a similar needle to the one used for taking a blood sample). The needle is attached to a syringe. A sample of cells or fluid from the lesion is collected. Fine-needle aspiration is a quick method to distinguish between a cyst and a solid mass. The collection of cells or fluid aspirated may be discarded or sent to University Health Network (UHN) in Toronto to be analyzed by expert pathologists. If the mass turns out to be solid you may require a core biopsy which is described below.
Ultrasound-guided core needle biopsy
This type of breast biopsy is used to assess a solid breast lesion that is visible on ultrasound. For the procedure, you will lie on a bed, and then under ultrasound guidance, the radiologist will locate the mass and will administer local anesthetic (freezing of the skin). A small incision is made in the skin to insert the needle. Several core samples of tissue (usually 3) are obtained and will be sent to University Health Network (UHN) in Toronto to be analyzed by expert pathologists.
Stereotactic core needle biopsy
This type of biopsy uses mammography to pinpoint the location of a suspicious area, usually calcifications, within the breast. You will either be sitting or lying on your side for this procedure. You may need to remain in this position for 30 minutes. Your breast will be firmly compressed between two plates. After an image is obtained, a computer will calculate the exact position to where the needle should go. The radiologist will administer local anesthetic (freezing of the skin), and will make a small incision in the skin to insert the needle into the area of concern. Several core samples of tissue (usually 5) are obtained and will be sent to University Health Network (UHN) to be analyzed by expert pathologists.
Magnetic Resonance (MR)-guided vacuum assisted
MR guided biopsy is performed when there is a suspicious or indeterminate finding on MRI with no corresponding finding on US or mammography. During this procedure you lie facedown on a padded scanning table similar to regular breast MR imaging. Your breasts fit into a hollow space in the table. The breast will be tightly compressed. A special computer program determines the exact location for the biopsy. The radiologist will administer local anesthetic (freezing to the skin), and will make a small incision in the skin to insert the needle into the area of concern. This biopsy is done with a vacuum system. The samples of tissue obtained will be sent to University Health Network (UHN) to be analyzed by expert pathologists.
After a breast biopsy
After the guided biopsy with ultrasound, stereotactic, or MRI, you'll go home with bandages over the biopsy site. It is beneficial to apply ice to the area. You should not do any strenuous exercise the day of your biopsy but otherwise you'll be able to resume your normal daily activities. Bruising is common after core needle biopsy procedures. A post procedure instruction sheet will be provided for you.
The pathology report will be sent to your Health Care Provider (HCP) within 7-10 days.
Pre-operative Needle-Wire Localization
The surgeon performing the excision biopsy schedules these procedures. The procedure is performed with mammography, ultrasound, or magnetic resonance guidance. The modality is pre-determined by the Radiologist at the time of the pre-operative workup. The skin will be cleaned; then local anesthetic is injected with a very fine neede. You may feel a slight sting. A localization wire is then inserted. Because of the local anesthetic, most patients report only minimal discomfort. Additional mammogram will be obtained after the procedure is done. You will be escorted to the Surgical Day Care. This is the holding area prior to your surgery.
Sentinel Node Injection
This is a surgical diagnostic procedure done to remove a small sample of lymph nodes from under the arm ( axilla ). A sentinel lymph node is defined as the first lymph node to which cancer cells are most likely to spread from a primary cancer.
A nuclear medicine specialist will inject a weak radioactive substance around your nipple. This can be painful. The surgeon then uses a device that detects radioactivity to find the sentinel node during your surgery.
Our Surgical Services include:
- Apirations
- Lumpectomy
- Mastectomy
- Sentinel node biopsy
- Axilllary Node Dissection